You'll Learn
- Hospital Linen Management: A Key to Infection Control
- Hospital Linen Management and Infection Transmission Risks
- 7 Proven Tips to Improve Hospital Linen Management
- How Can You Ensure Safe Linen Handling in Hospitals?
- FAQs on Infection Control in Hospital Linen Management
- Strengthening Hygiene Through Hospital Linen Protocols
Hospital Linen Management: A Key to Infection Control

Effective hospital linen management is critical for infection control in healthcare facilities. Every bed sheet, pillowcase, and medical gown has the potential to carry pathogens that threaten patient safety. That's why hospital linen management for infection control is a critical component of healthcare facility operations.
From surgical wards to recovery rooms, effective linen protocols help reduce the risk of healthcare-associated infections (HAIs), support regulatory compliance, and safeguard both patients and staff.
In this blog, we break down seven practical tips to help healthcare professionals, environmental services teams, and administrators optimize clinical textile handling and maintain the high standards of cleanliness. These insights not only reflect best practices for hospital linen management but also align with modern infection control standards and government health regulations.
Hospital Linen Management and Infection Transmission Risks
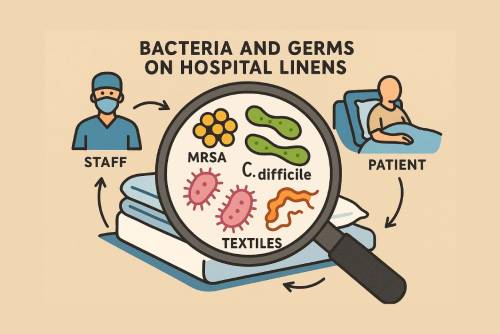
Hospital linens—including patient gowns, bedding, towels, and surgical drapes—can serve as silent carriers of infectious agents if not properly handled. Proper hospital linen management reduces the risk of pathogens spreading through textiles. Studies show that textiles exposed to bodily fluids or patient skin can harbour bacteria like MRSA, C. difficile, and other pathogens. If these fabrics are mishandled or improperly stored, they can become transmission points for infections.
Regulatory agencies such as the CDC, EPA, and OSHA emphasize stringent hospital laundry infection control protocols. That includes correct temperature settings, safe transport practices, and clean linen processing procedures.
Infection prevention doesn’t begin or end in the operating room. It extends throughout the laundry process, following the Definitive Guide to Laundry and Bedding Standards (2024) to ensure pathogen elimination via regulated temperature, PPE use, and transport.
7 Proven Tips to Improve Hospital Linen Management

Effective hospital linen management is essential for maintaining hygiene, reducing infection risks, and ensuring smooth healthcare operations. These seven proven tips—ranging from separating soiled and clean textiles to partnering with accredited laundry services—provide a practical framework for healthcare teams to follow.
Tip #1: Separate Clean and Soiled Linens

A cornerstone of hospital linen handling procedures ensures compliance with hospital linen management protocols. Cross-contamination can occur at any point if protocols aren't enforced.
How to Handle Soiled Linens in Hospitals
- Always treat used linens as potentially infectious.
- Use color-coded bags or carts to distinguish between clean and dirty laundry.
- Never place soiled linens on the floor or over clean surfaces.
- Fold soiled linens away from the body.
- Avoid shaking or agitating them, which can disperse pathogens into the air.
- Staff should always wear gloves when collecting used linens.
Linen cart disinfection is also critical. Ensure carts are wiped down with EPA-approved disinfectants after every use. Visual signage can reinforce clinical textiles handling procedures and minimize mistakes during peak hours.
Tip #2: Best Practices for Hospital Laundry Infection Control

Hospital laundry infection control begins in the laundry facility. Effective hospital laundry infection control ensures bedding is free of harmful bacteria. If your laundry unit doesn't meet disinfection benchmarks, it's undermining all other hygiene efforts.
Infection Control Laundry Tips
- Wash linens at temperatures above 160°F for a minimum of 25 minutes.
- Use EPA-registered laundry sanitizers to eliminate pathogens.
- Avoid overloading machines to ensure thorough agitation and rinsing.
HVAC Ventilation in Laundry Facilities

Proper ventilation systems reduce airborne contaminants in healthcare linen processing. An effective laundry ventilation system should include filtered airflow and negative pressure zones to contain potential bioaerosols. Implementing laundry facility infection risk assessments is essential to identify and address vulnerabilities.
Tip #3: Train Staff on Safe Linen Handling Procedures

Even the best procedures fall short without proper training. Routine sessions reinforce the importance of hospital laundry infection control and compliance. Linen protocols are only as effective as the people who follow them. Investing in staff training is a vital step in reducing risk and improving consistency across shifts.
Hospital Linen Management Guidelines

- Provide regular refresher training on the hospital's proper linen handling procedures.
- Reinforce safe linen handling in hospitals through visual aids and checklists.
- Conduct spot audits to ensure compliance.
Staff training should also align with gown usage protocols. For example, understanding why patient gowns are open back or when to choose medical gowns vs. coveralls helps reinforce PPE best practices, improving hygiene across all patient interactions.
Tip #4: Use PPE and Engineering Controls in the Laundry Facility

Those working in laundry and environmental services should be viewed as the first line of defense against the spread of germs. Equip them accordingly.
Personal Protective Equipment for Laundry Staff
- Waterproof gloves
- Face shields or goggles
- Gowns or coveralls
Healthcare linen processing requires PPE to protect staff from biohazards. These layers of protection reduce exposure to biohazards during healthcare fabrics processing.
Engineering Controls and Benchmarks
Implement barrier walls, hand-sanitizing stations, and automatic door systems to reduce contamination risks. Periodic linen audits and high-quality benchmarks help monitor whether standards are being upheld.
Tip #5: Maintain Proper Storage and Transport Protocols

Linens may be cleaned and disinfected perfectly, but if they’re stored or transported incorrectly, they can be re-contaminated.
Proper Linen Transport in Healthcare Facilities
- Use separate trolleys for clean and soiled bedding.
- Keep clean linen carts covered during transport.
- Follow defined traffic routes to prevent cross-flow between dirty and clean areas.
Linen Storage Area Cross-Contamination Control
Storage rooms should be cool, dry, and well-ventilated. Never store clean bedding and towels near trash bins or biohazard disposal. Environmental services teams play a key role in ensuring compliance with both transport and storage procedures.
Tip #6: Audit Your Healthcare Linen Management System

An effective way to identify gaps in your system is through periodic auditing. This ensures that your hospital linen management infection control plan evolves with best practices and regulatory changes.
Linen Audits and Quality Benchmarks
- Track linen loss rates, rewash frequency, and reject loads.
- Monitor infection rates to identify potential breaches in fabric hygiene.
- Conduct laundry facility infection risk assessments quarterly.
These audits improve transparency, promote accountability, and build trust with accreditation bodies. Healthcare linens are often an overlooked vector in HAI outbreaks—from mold to MRSA. A detailed review titled Top Healthcare Linen Infection Risks (2024 insight) reinforces the necessity of proactive quality control and periodic auditing.
Tip #7: Partner with Accredited Healthcare Laundry Services

Outsourcing can be beneficial, but only if the partner meets or exceeds internal hygiene standards.
Choosing Accredited Laundry Vendors
- Look for HLAC, TRSA, or ISO certification.
- Evaluate their adherence to OSHA, EPA, and CDC regulations.
- Verify that they conduct regular internal and external audits.
Questions to Ask Providers:
- What disinfection protocols do you use?
- How do you ensure clean textile processing?
- Can you provide documentation on linen management benchmarks?
Working with an experienced provider not only ensures compliance but also frees up your internal team to focus on patient care.
How Can You Ensure Safe Linen Handling in Hospitals?
This is one of the most common questions among infection control teams.

Checklist for Safe Linen Handling
1. Staff wear PPE and follow handling protocols.
2. Soiled and clean linens are separated at every stage.
3. Storage and transport areas are secure and hygienic.
4. Laundry operations follow disinfection and ventilation requirements.

Common Mistakes to Avoid
1. Reusing linen carts without disinfection.
2. Storing clean linens near contaminated equipment.
3. Inadequate staff training or failure to update protocols.
FAQs: Coffee Machines

Q1: What are the best practices for hospital linen management?
Separate laundered items by contamination level, follow disinfection protocols, store properly, and train staff regularly.
Q2: How often should hospital linens be changed to prevent infection?
Change textiles after each patient discharge, or daily for inpatients, depending on facility protocol and patient risk.
Q3: What type of PPE is needed for laundry staff?
Gloves, gowns, masks, and eye protection to minimize contact with biohazards.
Q4: Can you sanitize hospital linens without high-temperature water?
Yes, but only with EPA-approved disinfectants and specific chemical protocols. Thermal disinfection remains the gold standard.
Q5: How do I choose a reliable healthcare laundry service?
Look for certifications (like HLAC), strong auditing procedures, and alignment with federal and provincial healthcare regulations.
Strengthening Hygiene Through Hospital Linen Protocols

Hospital linen management infection control is more than just a laundry concern. It’s a foundational part of hospital hygiene and patient care. From training staff to partnering with accredited providers, each tip we shared contributes to lowering the risk of HAIs and ensuring compliance with modern healthcare standards.
Take the next step by conducting an internal audit, updating your hospital linen handling procedures, or scheduling a vendor review. For deeper guidance, explore our related content on:
Together, these resources form a comprehensive guide to improving textile hygiene in your healthcare facility.
- Hospital Gown Colors Meaning: 5 Surprising Insights
- Why Patient Gowns Are Open-Back
- Medical Gowns vs Coveralls
Stay safe. Stay compliant. Stay clean.

